FEMALE FERTILITY PROBLEMS
Female Fertility Video
Basic examinations to diagnose female fertility
Approximately 15% of couples do not conceive after 12 months of unprotected, regular sex[1]Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Human Reproduction. 2003. … Continue reading. By this stage, women have usually discussed their desire to have children with their GP or gynecologist during their routine examination. They should do so especially if they have reason to be concerned about their fertility, for example if they have had treatment for cancer, or if they are over 35.
About 40% of the issues involved with infertility are due to the woman, another 40% due to the man, and 20% result from complications with both partners[2]Hudson B. The Infertile Couple. 1987. Churchill-Livingstone, Edinburgh.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
Fertility testing and investigation can be a lengthy process, and female fertility decreases with age, so it is best to discuss this early on. The process of trying to conceive can be emotional, so it is important to get as much support as possible. Stress is just one of the many things that can affect fertility. With the aid of a few quite simple questions and tests, the GP or gynecologist can determine possible fertility disorders in women and set the couple off on the right “fertility path”.

Medical, sexual and social history
When a woman visits her GP or gynecologist to enquire about her fertility, the doctor will want to discuss her full medical, sexual and social history. This will help him or her identify what may be causing fertility problems.
Age
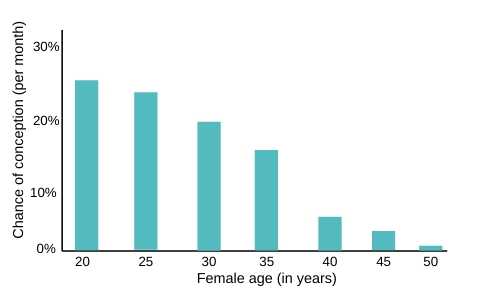
Natural fertility in women rapidly declines with age, and the doctor will evaluate the chances and risks of a pregnancy based on the couple’s age profile.
Children
The doctor will discuss any previous births and any related complications with previous pregnancies. The doctor will also ask about any miscarriages.
Irregular menstrual cycles
If the woman’s cycles are longer than on average, mathematically she may only ovulate every six weeks or about nine times a year. She will therefore have fewer opportunities to conceive. This is a statistical disadvantage in a numbers game of probabilities.
For this reason, women with long cycles are sometimes given fertility drugs like Clomid to regulate ovulation. Women over 35 and don’t ovulate regularly are the most likely candidates for drug therapy.
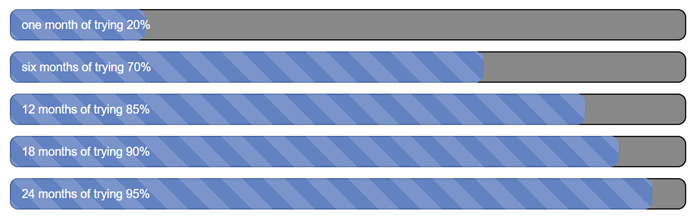
Length of time trying to conceive
The GP will ask how long the couple has been trying to conceive. This graph shows the average percentage of fertile couples achieving pregnancies after[3]Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Human Reproduction. 2003. … Continue reading:
Sex
Couples may be asked how often they have sex, and whether they have any difficulties during sex. They may feel uncomfortable or embarrassed about discussing their sex life with their doctor.
However, it is very important to be open and honest. If the fertility problem is caused by sexual potency or motivation, this might be easily overcome.
Time since stopping contraception
The couple will be asked about the type of contraception they previously used, and when they stopped using it. It can sometimes take a while for certain types of contraception to stop working, and this may be affecting current fertility.
Medical history and symptoms
The doctor will discuss any medical conditions the couple may have, or have had in the past, including sexually transmitted infections (STIs). The doctor may also ask:
Medication
The side effects of some medications can affect female fertility. The doctor will look at any medication the woman is or has been taking, and might discuss alternative treatments. She should mention any non-prescription medication she is taking, including herbal medicines.
Habits
Several lifestyle factors can signifcantly affect fertility. The GP will want to know:
The doctor may recommend changes to the couple’s lifestyle to increase their chances of conceiving.

Basic physical examinations and tests
After discussing the couple’s medical, sexual and social history, they may be referred to a fertility specialist for further tests and procedures.
Physical tests
The doctor will also examine the woman’s pelvic area for clues about possible problems. Checking for infection, lumps or tenderness, which could be an indication of fibroids, ovarian tumours, endometriosis or pelvic inflammatory disease (PID).
Hormone tests
Blood tests taken at various times in the cycle can provide clues about fertility problems.
The female’s blood may be tested for progesterone, to check whether she is successfully ovulating. The timing of the test is based on how regular her periods are. If she has irregular periods, she will be offered a test to measure messenger hormones called gonadotrophins, which stimulate the ovaries to produce eggs.
It is also often advantageous to regularly measure the classic parameters of FSH, LH, oestrogen and progesterone, as well as controlling a variety of other factors such as the regular functioning of organs. This is because even slight hypothyroidism can be responsible for disruptions in a woman’s cycle[4]Weiss RV, Clapauch R. Female infertility of endocrine origin. Arq Bras Endocrinol Metabol. 2014. 58(2): 144-52.
Checking the ovaries
The women’s ovaries will be tested before she is offered fertility drugs. This may done via a blood test to measure certain hormones or an ultrasound scan to examine the follicles in the ovaries.
30%
of infertile couples are affected by ovarian conditions
Chlamydia test
Chlamydia is an STI (Sexually Transmitted Infection), which can affect fertility. The gynecologist or sexual health specialist will take a swab (similar to a cotton bud, but smaller, soft and rounded) to collect some cells from the cervix to test for chlamydia.
If chlamydia is diagnosed, prescription antibiotics can effectively treat it. During this session other standard checks will be performed including for herpes, gonorrhoea, syphilis and HIV using urine and blood samples.
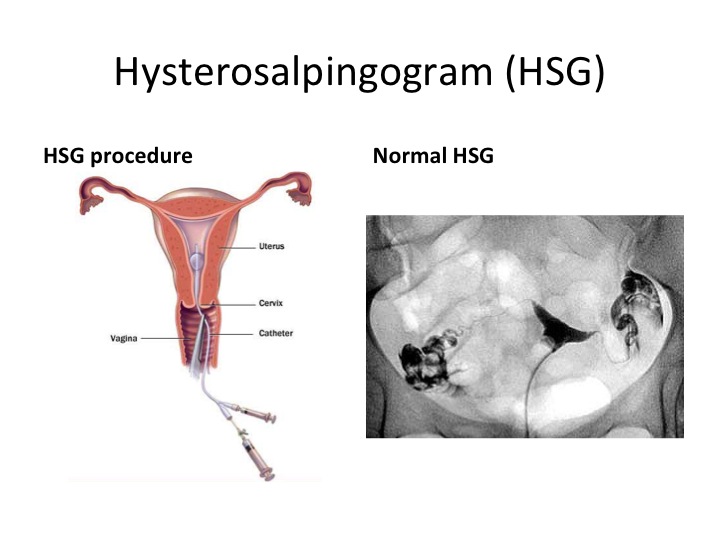
Hysterosalpingogram
A hysterosalpingogram (HSG) is a type of X-ray taken of the womb (uterus) and fallopian tubes after a special dye has been injected. This will outline the cavity of the womb and detect any blockage of the fallopian tubes.
25%
of infertile couples are affected by tubal diseases
In addition to the endometriosis conditions such as fibroid and polyps, adenomyosis can also lead to the obstruction of the uterus and Fallopian tubes. A pap smear, which can be conducted during a routine gynaecological investigation, can be used to diagnose bacterial infections, fungal infections or cell changes, which in some cases can indicate a disorder affecting fertility.
Most doctors conduct an HSG ultrasound scan as part of the first fertility diagnosis. This helps with the detection of myomas, endometriosis and malformations of the uterus. The HSG will also visually represent the development of maturing follicles and the construction of the endometrium for examination.
10%
of infertile couples are affected by endometriosis
If no fertility disorders are discovered in these first investigations, the male partner should have his sperm checked via a semen analysis, if this has not already been done.
Some doctors may also recommend a post-coital test at this point[5]Hessel M, Brandes M, de Bruin JP, Bots RSGM, Kremer JAM, Nelen WLDM, Hamilton CJCM. Long-term ongoing pregnancy rate and mode of conception after a positive and negative post-coital test. Acta Obstet … Continue reading.
3%
of infertile couples are affected by problems with the female cervical mucus
Further investigations into female fertility
However, it may still be the case that no fertility problems are found. At this point, fertility specialists may recommend a hysteroscopy or a laparoscopy as a next step to diagnose the fertility problem.
Bibliography

Dr. Kooner is Deputy Director of The Advanced Fertility Center of Chicago and has been a Specialist in Fertility Treatment since 1999.
As well as the areas that the clinic specialises in general, he is particularly interested in managing oocyte donation, female same-sex couples, single women having sperm donation and those considering egg freezing.
Dr. Kooner regularly speaks at fertility meetings. He has published in national journals and constantly contributes to the fertility research and publications from Advanced Fertility Center of Chicago.
References
| ↑1, ↑3 | Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Human Reproduction. 2003. 18(9): 1959-66 |
|---|---|
| ↑2 | Hudson B. The Infertile Couple. 1987. Churchill-Livingstone, Edinburgh |
| ↑4 | Weiss RV, Clapauch R. Female infertility of endocrine origin. Arq Bras Endocrinol Metabol. 2014. 58(2): 144-52 |
| ↑5 | Hessel M, Brandes M, de Bruin JP, Bots RSGM, Kremer JAM, Nelen WLDM, Hamilton CJCM. Long-term ongoing pregnancy rate and mode of conception after a positive and negative post-coital test. Acta Obstet Gynecol Scand. 2014. 93(9): 913-20 |




So I was pregnant and I had a ectopic pregnancy And they took one of my tubes out and they took the baby out And I am 18 how do I get my body right and in got shape so this won’t happen again
Hi
My husband all reports are good , I have mild pcod but after hormone injection , it become good . My periods are normal ,doesn’t miss any month and intercourse will be done as doctor suggested but after all that periods will come.
My I know where it is going work..