
Methodology
An IVF procedure involves a woman’s eggs being removed from her ovaries. The eggs are then fertilised by sperm cells in a laboratory, which results in the formation of an embryo. This is placed inside the woman’s uterus. Before this procedure, a woman may need a take fertility drugs to encourage egg cells to be released. In some cases, donor eggs and/or donor sperm are necessary.
When is IVF recommended?
IVF is usually considered as an option by couples who have:
- Blocked or absent fallopian tubes
- Male factor infertility (in some cases a sperm donor may be necessary)
- Attempted other fertility treatments such as IUI or ICI without success
- Tried fertility drugs without success
- Unable to conceive despite actively trying for over twelve months
- Advanced reproductive age where conception time is critical and success rates with other therapies are generally low
- Ovarian failure (would require donor eggs)
- Other infertility causes where no treatment is successful (such as ovulation disorders, endometriosis, and unexplained infertility).
- Or are in a homosexual relationship
Pre-treatment checks
Prior to consideration of IVF treatment a series of screening tests are preformed. This initial consultation will include taking full medical history of both partners with particular focus on fertility factors. This can include timing of intercourse, menstrual history, previous pregnancy history, any sexual dysfunction issues, semen parameters. Screening for some genetic conditions is also available and can be discussed with your fertility specialist.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
Common pre-pregnancy screening tests may include:
- Chicken pox immunity
- Rubella (German measles) immunity
- Syphilis serology
- HIV
- Hepatitis B and C
- Blood group and antibody status
- Full blood count
- Current breast check and pap smear (within the past two years)
During a basic fertility assessment a pelvic ultrasound and ovulation testing is performed. Hormone levels are also measured. In some cases other gynaecological investigations may be necessary. This is usually the case for women with medical conditions such as PCOS or endometriosis, or of advanced maternal age. Specialist blood test may be requested to determine egg reserves, or special ultrasounds to assess tubal patency.
- HIV
- Hepatitis B and C
A standard semen analysis will also be preformed. This will investigate sperm count, concentration, motility and morphology. In some cases, a physical examination and blood tests will also be requested.
* It’s very important not to underestimate the male role in IVF. Prior to undertaking IVF treatment, men can take important steps to improve their chances of starting a family. Ensuring that your sperm is as healthy as it can possibly be can significantly improve conception rates. Sperm takes three months to fully mature and during this time you can influence sperm health through positive lifestyle changes. Exercising, not smoking, avoiding stress, and drinking alcohol in moderation can support healthy sperm development. Nutrition is particularly important.
Learn more about the importance of diet for male fertility
Key nutrients for male fertilityOften a follow-up consultation is required to discuss the results of pre-pregnancy screening tests. During this appointment, your fertility specialist will provide you with a detailed recommended treatment plan and give you an indication of your pregnancy chances. The chances of successful conception can range from between 5% and 50%, based on:
- Any pre-existing medical conditions
- How long you have been trying to actively concieve
- Your age
- Your partner’s age
- Whether either of you already have already had children
- If previous fertility treatment(s) has been sought
*Please note – In some countries, legislation requires that both patients undergo a police and child protection order check before commencing IVF treatment
Procedure steps
IVF is one of the most complicated ARTS procedures. It involves multiple steps that occur over several weeks. These include:
- Ovarian stimulation for egg production
- Egg retrieval from the ovaries
- Obtaining a semen sample
- Laboratory fertilisation of the eggs with the sperm
- Embryo growth in a laboratory
- Transfer of one of more developing embryos into the uterus
Usually more than one IVF treatment is required before a successful pregnancy. In some cases, women will not fall pregnant despite multiple IVF cycles.
Step 1: Ovarian Stimulation
The first stage of IVF involves fertility medications. These are taken to help increase the number of follicles that form within the ovaries by regulating hormones[1]“Macklon, N. et.al. (2006). The science behind 25 years of ovarian stimulation for in vitro fertilization. Endocrine Review. Volume 27, Issue 2, (pp. 170).”. This medication also helps to control ovulation timing.
There are a range of fertility medications available. The most popular include clomiphenes citrate, metformin hydrochloride, and gonadotrophins. The medication selected will depend on the physician’s preference and the woman’s individual diagnosis.
Often fertility medications are given as injections rather than orally. Women are shown how to inject the medication daily under the skin so that they can take the medication at home without having to attend a clinic.
After several days of injections, blood tests are taken to determine hormone levels and a pelvic ultrasound is often required to assess follicle growth. Depending on the results, fertility medication does may be increased or decreased. Often these tests are preformed several times throughout a cycle.
The aim of fertility medication is to produce a least two healthy follicles that are around 15-18 mm in length. In many cases, much more than two follicles develop. Once healthy follicles have been identified as ‘ready’, human chorionic gonadotropin (hCG) is injected to stimulate ovulation. Approximately 36 hours later, the follicles will be prepared for the egg retrieval process.
In some cases, it is possible to perform unstimulated IVF without the use of fertility medications. However, this is a rare practice and the majority of IVF procedures worldwide use from form of ovarian stimulation.
Step 2: Egg Retrieval
Following a hCG injection a specialised procedure is performed for oocyte removal. This usually occurs between 32 and 36 hours after the hCG injection. The physician uses an ultrasound probe inserted into the vagina to remove eggs from the follicles using a specialised needle. Sedation is often used during the procedure and it can take up to 30 minutes depending on the number of eggs retrieved.
Women can usually go home the same day after several hours in recovery. However, due to the use of anaesthesia driving is not advised.
Step 3: Embryo Transfer
Between two and five days after the eggs have been retrieved and fertilised, one of more embryos are inserted into the uterus. This process is done using a flexible, thin catheter inserted through the woman’s cervix. This process is done as gently as possible to reduce uterine cramping. Generally, anaesthesia isn’t necessary for embryo transfers.
Following the procedure, the patient is encouraged to rest for several hours. Progesterone medication may be prescribed to improve the probability of embryo implantation in the uterus. Often this medication is taken on the retrieval day or transfer day. It may be administered as a suppository, vaginal gel, or an injection into a muscle.
Providing a Semen Sample
Although the majority of IVF processes involve laboratory processes and focus on successful egg retrieval and embryo transfer, the male role in this ART is also critical. The provision of healthy, viable sperm is essential for fertilisation.
There are three main ways sperm is provided for IVF:
Ejaculation
This is the most common way to obtain semen for IVF. It is usually done by masturbation and collection of the day of egg retrieval. To ensure an optimum quality sample, there are a few measures men can take including:
- Abstain from ejaculation for a minimum of two days but no longer than five days prior to collecting a semen sample.
- Semen must be collected in a non-toxic, sterile, plastic container provided by the fertility clinic
- Lubricants should be avoided unless stated otherwise by your physician
- Generally clinics prefer that a specimen is collected on site in a private collection room. Hands should be washed and dried before collecting semen to prevent contamination.
- Some clinics will allow a semen sample to be collected at home, although the specimen container must be kept at body temperature and delivered to the IVF clinic within two hours of providing the sample.
- Always follow the clinics instructions for transporting and labelling the specimen.
- If you have any difficulties collecting a sample, this should be discussed with your physician to determine if an alternative method could be used.
In some instances, fertility specialists will recommend cryopreservation of a semen sample several days before the egg retrieval procedure. This frozen sample can be used as a ‘back-up’ in case there are problems with the semen sample on the day of egg extraction. Also, some fertility specialist will recommend that men take antibiotics before semen collection for IVF.
TESE / TESA
TESE (testicular sperm extraction) and TESA (testicular sperm aspiration) are surgical procedures used to extract sperm directly from the testes. These processes may be necessary when spermatozoa numbers are exceptionally low or there is a sperm transport obstruction that is preventing sperm from entering the ejaculate.
Learn about sperm transport obstructions
Sperm Donor
Also known as heterologous insemination, a sperm donor can be beneficial in the following situations:
- If the male partner is unable to produce sperm or no sperm can be collected through TESE/TESA.
- If testes have been surgically removed.
- Following radiation or chemotherapy that has resulted in infertility.
- If the man carries a genetic disorder that parents don’t want passed down to their children.
- Lesbian couples seeking to have IVF treatment to start a family.
Step 1: Semen Preparation
While eggs are being retrieved, semen is being prepared in the laboratory. How semen is prepared will depend on the quality of the sample and the procedures adopted by the specific clinic. The most common procedure is called density gradient preparation. Semen is added to a special media within a test-tube that removes sperm with poor motility. In the case where surgical sperm collection sperm was needed, or sperm count is low, the semen sample may undergo a spinning procedure to concentrate the sperm.
Step 2: Insemination
Insemination techniques may vary. Following egg retrieval, often the oocytes are combined in a laboratory dish with sperm and left overnight to fertilise. Generally, half the oocytes will become fertilised. This is the standard IVF insemination procedure used for patients with normal semen parameters. However, if sperm parameters are abnormal, or previous standard IVF insemination has failed, other methods may be adopted. Usually this involves combining IVF with ICSI, whereby technicians manually fertilise eggs with sperm. Fertilisation rates using ICIS can vary from between 50 and 70%[2]“van Rumste, M. et.al. (2003). Intra-cytoplasmic sperm injection versus conventional techniques for oocyte insemination during in vitro fertilisation in patients with non-male subfertility. … Continue reading.
Read more about ICSIStep 3: Fertilisation and Embryo Culture
The next day following insemination, the eggs are checked for signs of fertilisation.
If fertilisation is successful and embryos are evident, they are then grown further in the lab. How long the embryos grow before transfer into the uterus will depend on your fertility specialist and the agreed IVF procedure. Some clinics offer different stages of embryo culture prior to transfer. Depending on the clinic, embryos may be received at the cleavage of blastocyst stage. Embryos two or three days old are at the cleavage stage. This stage is usually offered to couples with a low number of available embryos for transfer. Embryos four or five days old are typically more developed and at the blastocyst stage. This stage may be offered to couples with more embryos available than they want to have transferred. It allows scientists to select the most developed embryo for transfer.
Duration
Each IVF cycle takes approximately four to six weeks. The lengthiest process is waiting for follicles to mature. On the day of IVF treatment, both partners will spend approximately half the day at a clinic. During this time, a semen sample will be collected and prepared, and eggs will be retrieved ready for fertilisation. Approximately two to five days later, embryos will be inserted into the uterus back at the clinic.
Many fertility clinics sell IVF in multi-cycle packages. While it was previously thought that consecutive IVF treatments were detrimental to subsequent cycles, more recent research suggests otherwise[3]“Kolibianakis E, et.al. (2002). Effect of repeated assisted reproductive technology cycles on ovarian response. Fertility Sterility. Volume 77, (pp. 967-970).. Consequently, many couple choose two or three-cycle IVF packages at a discounted rate. Some clinics may offer a partial refund if conception is achieved in the first cycle.
Success rate
The success rate for IVF procedures can be variable. A lot of factors influence conception chances. On average, there is a 35% chance of conceiving and a 28% chance of delivering a baby with every IVF cycle. The younger a woman is, the healthier her eggs and the greater the chance of success.
HFEA published data (on 19/5/2014) for the period 1st July 2012 – 30th June 2013 (For fresh IVF & ICSI cycles)
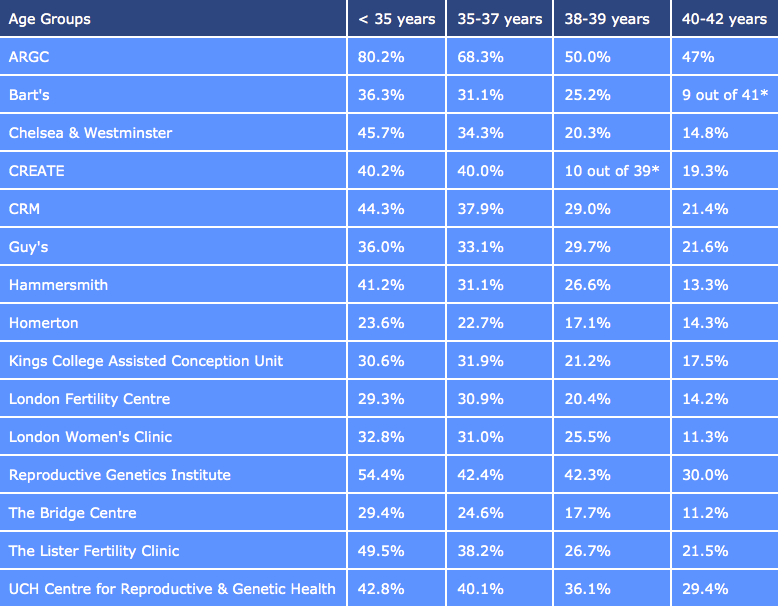
It’s important to note that even women under the age of 35 may still struggle to conceive within the first IVF cycle. In a Swedish study, it was observed that women who underwent three cycle of IVF had a 66% chance of conceiving[4]“Olivius, C. et.al. (2002). Cumulative probability of live birth after three in vitro fertilization/intracytoplasmic sperm injection cycles. Fertility and Sterility. Volume 77, Issue 3, (pp. … Continue reading. This was much higher than couples that only undertook one or two cycles. However, financial constraints may be a limiting factor in facilitating multiple cycles for many couples. Psychological stress has also been identified as a reason why many couples cease participating in IVF cycles[5]“Olivius, C. et.al. (2002). Why do couples discontinue in vitro fertilization treatment? A cohort study. Fertility and Sterility. Volume 81, Issue 2, (pp. 258-61).”.
Enhancing probabilities
If you have been pregnant or have had a baby in the past, you have a higher chance of IVF success. However, for hopeful first-time parents there are other measures you can take to improve your chance of success.
- Maintaining a healthy body weight is important. A body mass index (BMI) between 19 and 25 is ideal.
- Alcohol consumption should be limited to one unit per day, or completely avoided.
- Cease smoking.
- Reduce caffeine intake.
- Increase vitamin D and foliate intake.
A healthy diet is very important for conceiving and supporting a healthy pregnancy.
Learn More
Key nutrients for female fertilityCost of IVF
NHS (FREE)
In some circumstances the NHS may provide funding for IVF treatment in the UK. You must have a referral from your doctor to access NHS funding. This requires meeting certain criteria as set out by the relevant governing organisations in the UK.
If eligible, there are waiting times before IVF cycles can commence and these times will vary depending on the clinic. Currently in England, many clinics have an ‘eighteen week policy’. This means that the time of your referral to starting the IVF treatment should be within eighteen weeks.
Although IVF funding may be available through the NHF, often couples still have to pay for the prescription charges associated with fertility medications.
For specific IVF funding eligibility criteria in your location, it’s recommended that you first consult your local doctor.
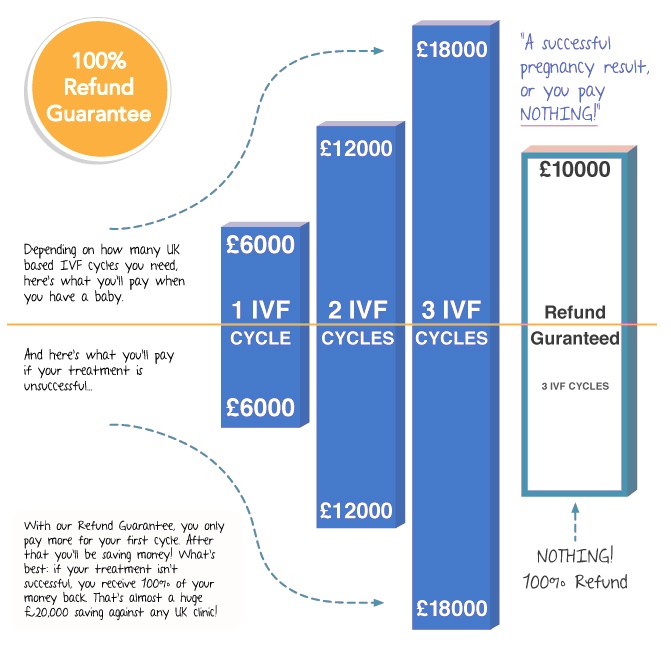
UK IVF REFUND SCHEME
 InterTrust Fertility in the UK offers patients a refund programme on 3 full IVF cycles, plus the guarantee of a full refund for approximately the same cost of a single IVF cycle in the UK.
InterTrust Fertility in the UK offers patients a refund programme on 3 full IVF cycles, plus the guarantee of a full refund for approximately the same cost of a single IVF cycle in the UK.
Normally in the UK patients don’t receive any form of guarantee.
InterTrust do this through an IVF clinic in Prague, where the cost of treatment so approximately 50% less than in the UK. They will also be able to claim refunds from the NHS.
This allows InterTrust to offer patients a refund of the full cost of treatment, if three cycles (either with their own eggs or a donor’s eggs) are unsuccessful, minus the cost of their medications.
The eligibility criteria are detailed, but this programme makes IVF treatment more accessible to patients, because it removes the risk of large debts following unsuccessful treatment.
How does the InterTrust IVF Refund Scheme for UK residents work?
PRIVATE
There are many private clinics throughout the UK that offer IVF treatments. However, their prices are not regulated and can vary considerably. Often clinics will offer multi-cycle packages to increase conception success rates.
It’s important to ask exactly what is covered in the price and what other expenses you may need to allow for. Generally fertility medications are not factored into the price of private IVF cycles. You should also consider any costs for medical reports, counselling, consultations, tests, scans, and any other necessary processes.
The average cost per IVF cycle usually falls within the range of £5,000 and £10,000.
There are current scientific developments underway to reduce the expensive of IVF cycles. However, how successful these will be and when they may become available is still unknown.
Learn more about the cost of treatment in your region
Select your locationFertility Tourism
Many couples choose to seek fertility treatment abroad due to lower costs. In some countries, IVF treatments cost much less than the price of having the same treatment at home. This includes factoring in other expenses such as accommodation and flights. See below for a general price comparison.
Average cost of a single cycle of IVF
| Country | USD | GBP | EURO |
| Brazil | $4000 | £2,525 | €3030 |
| Czech | $2,965* | £1,870 | €2250 |
| Greece | $3,900-$4,300 | £2,500- £2,800 | €3,000-€3,350 |
| Hungary | $2,350 | £1,500 | €1800 |
| India | $2,000 – $3000 | £1,265- £1,895 | €1,525- €2,285 |
| Lithuania | $1,982 | £1,275 | $1,506 |
| Russia | $3,150 | £2,000 | €2400 |
| Spain | $5,500-$6,500 | £3,500- £4,150 | €4,200-€5,000 |
| Turkey | $2,000 | £1,250 | €1500 |
| Ukraine | $1,825 | £1,150 | €1385 |
Source: https://fertility.treatmentabroad.com/costs
If you are going to consider undergoing IVF in another country, it’s very important that you fully research your options. You must comply with the rules and regulations set out by the country providing the fertility treatment.
Risks
It is important to note that although IVF has a high success rate, there are some disadvantages. Not only is IVF expensive, it also comes with the risk of complications as a result of the fertility drugs used and the invasive procedures used. Multiple gestation (twins, triplets) are a possibility, as well as premature births. Sometimes ectopic pregnancies may occur, however the risk is much lower compared with other fertility treatments.
It’s important to discuss all aspects of IVF treatments with your healthcare provider. Cover everything including benefits, risks and alternative before commencing treatment. In some cases, multiple cycles of less invasive and less expensive fertility treatment may be an option.
Bibliography

Dr. Kooner is Deputy Director of The Advanced Fertility Center of Chicago and has been a Specialist in Fertility Treatment since 1999.
As well as the areas that the clinic specialises in general, he is particularly interested in managing oocyte donation, female same-sex couples, single women having sperm donation and those considering egg freezing.
Dr. Kooner regularly speaks at fertility meetings. He has published in national journals and constantly contributes to the fertility research and publications from Advanced Fertility Center of Chicago.
References
| ↑1 | “Macklon, N. et.al. (2006). The science behind 25 years of ovarian stimulation for in vitro fertilization. Endocrine Review. Volume 27, Issue 2, (pp. 170).” |
|---|---|
| ↑2 | “van Rumste, M. et.al. (2003). Intra-cytoplasmic sperm injection versus conventional techniques for oocyte insemination during in vitro fertilisation in patients with non-male subfertility. Cochrane Database System Review.” |
| ↑3 | “Kolibianakis E, et.al. (2002). Effect of repeated assisted reproductive technology cycles on ovarian response. Fertility Sterility. Volume 77, (pp. 967-970). |
| ↑4 | “Olivius, C. et.al. (2002). Cumulative probability of live birth after three in vitro fertilization/intracytoplasmic sperm injection cycles. Fertility and Sterility. Volume 77, Issue 3, (pp. 505-10).” |
| ↑5 | “Olivius, C. et.al. (2002). Why do couples discontinue in vitro fertilization treatment? A cohort study. Fertility and Sterility. Volume 81, Issue 2, (pp. 258-61).” |



