Methodology
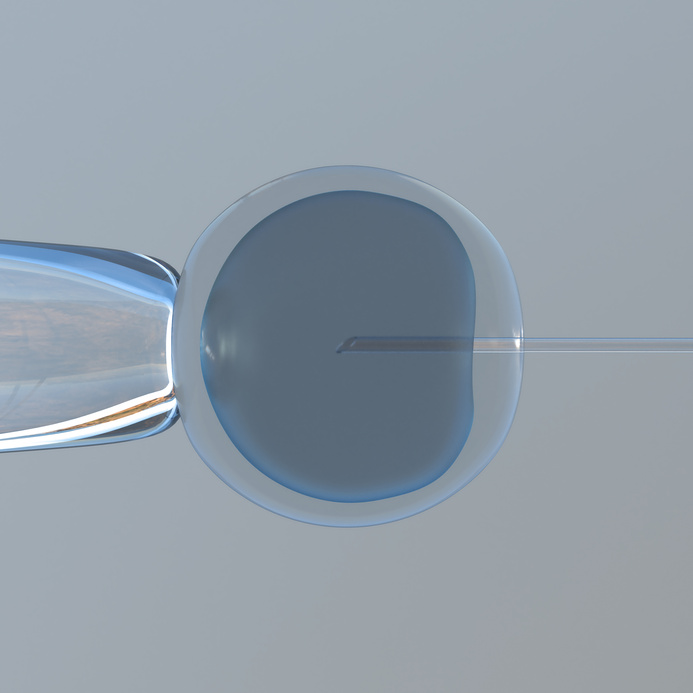
Intra-cytoplasmic sperm injection (ICSI) is a procedure that involves a single sperm cell being carefully injected into an individual egg cell. This is then placed in a woman’s uterus. The sperm may need to be removed from the partner or donor using a needle or biopsy, but this procedure usually results in only minor discomfort.The advantage of ICSI is that even if very few sperm are available, as long as some can be obtained, fertilisation may be possible.
When is ICSI recommended?
There are a range of reasons why people may consider intra-cytoplasmic sperm injection:
- When the male partner has a very low sperm count
- If a sperm analysis identifies other problems such as poor motility and/or abnormal morphology.
- If the sperm count zero and insemination by a donor is not wanted.
- If antisperm antibodies are preventing healthy sperm development
- When the male partner has undergone a vasectomy and sperm has been collected from the epididymis or testicles.
- When a vasectomy reversal procedure has been unsuccessful
- When the male partner has an erectile dysfunction. This may include men with diabetes, spinal cord injuries, and other disorders.
- If previous in vitro fertilisation (IVF) were unsuccessful or there was unexpectedly low fertilisation rate
Pre-treatment checks & procedures
In any ART treatment a series of tests are carried out to ensure that the procedure is suitable. This usually involves evaluating medical history and a range of physical tests.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
ICSI is very similar to in vitro fertilisation (IVF). The main difference is that instead of fertilisation occurring independently within a dish, sperm is carefully selected from a sample by an embryologist and injected directly into the eggs.
The ICSI pre-treatment checks and procedures leading up to the laboratory stage and following fertilisation are basically the same as for IVF.
The following 3D video provides a simple overview of ICSI and how it can help to achieve a healthy pregnancy.
Duration
It takes approximately four to six weeks to complete a ICSI cycle, similar to IVF cycles.
Success rate
The success rates for ICSI procedures are comparable with conventional IVF. Most clinics combine the statistics for both IVF and ICSI because the procedures are almost identical.
Enhancing probabilities
Being as healthy as possible in the lead-up to, and during a ICSI procedure, can help to increase the chances of a successful pregnancy. Eating well, getting enough sleep, and exercise are all important factors. Quitting smoking, not drinking alcohol, avoiding stress, and other positive lifestyle choices are also important. Paying close attention to diet can be a big influence on the success of ICSI as nutrition significantly influences egg, sperm and embryo development.
Costs
Couples choosing to undergo ICSI have the option of private treatment or the NHS. To qualify for NHS certain pre-requisites must be met. Due to the costs associated with ICSI, often couples consider traveling to another country where the prices are much lower. As ICSI is a form of IVF, the costs are similar.

Dr. Kooner is Deputy Director of The Advanced Fertility Center of Chicago and has been a Specialist in Fertility Treatment since 1999.
As well as the areas that the clinic specialises in general, he is particularly interested in managing oocyte donation, female same-sex couples, single women having sperm donation and those considering egg freezing.
Dr. Kooner regularly speaks at fertility meetings. He has published in national journals and constantly contributes to the fertility research and publications from Advanced Fertility Center of Chicago.



