Intracervical and Intrauterine Insemination (ICI and IUI)
Methodology
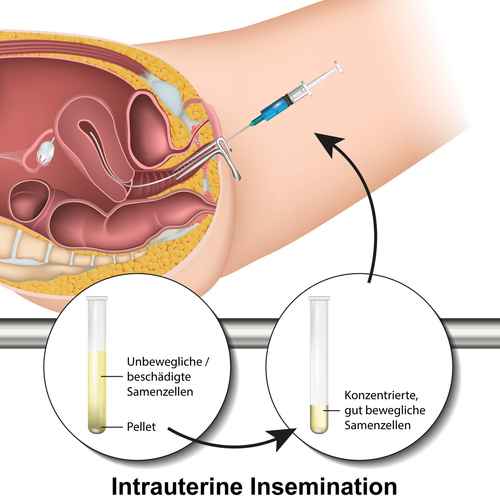
Intracervical insemination (ICI) and intrauterine insemination (IUI) are the most commonly used ARTs. ICI is the injection of semen into the cervix, while IUI injects the semen directly into the uterine cavity. ICI is the easiest and most common insemination technique, followed by IUI.
During ICI procedures, fresh, untreated or raw semen must be allowed to liquefy (read our article on liquefaction time) before it is sucked into the syringe. Alternatively, the syringe may be back-loaded, which will require additional specialist instruments.
In the case of IUI, the sperm must be prepared. This process known as “washing”, involves separating high quality (fast moving) sperm from poorly or non-moving sperm in a laboratory. If unwashed sperm is used uterine camping may result. This can cause discomfort and expel the sperm. Unlike ICI, instead of using a specialised syringe, a catheter is used to deliver sperm into the uterus.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
The ICI process is the simplest artificial insemination technique and closely replicates natural insemination by orgasm during intercourse. This is because fresh semen is deposited onto the neck of the cervix, the lower part of the uterus. Procedures for IUI are slightly more complicated because the sperm must be washed and inserted further into the uterus.
When is it recommended
The GP or fertility specialist may recommend intrauterine or intracervical insemination if:
- The couple have been trying for more than 12 months without success and there is therefore unexplained infertility
- The female partner has diagnosed ovulation problems
- The male partner is unable to fertilise the female egg by natural insemination, for example if he experiences impotence or premature ejaculation
- If the male partner experiences suboptiomal sperm quality following a series of semen analyses or if he experiences idiopathic (unexplained) infertility.
- The female does not have any known fertility problems but she may not have a male partner and is trying for a baby using donated sperm.
- If the couple is homosexual
Pre-Treatment Checks
The IUI/ICI approach requires a healthy female reproductive apparatus, especially open and healthy fallopian tubes. Before the IUI/ICI process begins, tubal potency test and a pelvis health checks are usually carried out by means of a laparoscopy and dye testing. This procedure is performed under a short general anaesthetic.
During the laparoscopy a telescope is inserted into the abdomen via keyhole surgery. This involves a small cut to the abdominal area, which will allow a direct view of the pelvis. Next, dye will be inserted into the uterus, which can be observed via an ultrasound scan. If the uterus and tubes are healthy, the dye can be seen to pass freely through both fallopian tubes.
There must be no adhesions present that might prevent an egg from having access from the ovaries to either fallopian tube. The test may show that the woman only has one open and healthy fallopian tube, although she may have both ovaries.
IUI/ICI treatments can only be carried out when there is evidence that ovulation is able to occur naturally and completely from the ovary that is on the same side as the open tube.
For IUI/ICI to be successful, inseminations must be preformed prior to or at the time of ovulation. To determine when a woman is ovulating the menstrual cycle is carefully monitored. This involves natural fertility checks such as measuring the basal body temperature and assessing the development and quality of cervical mucus.
Gynaecological sonograms or ovulation predictor kits can also be utilised. Urine or blood test may be performed to determine luteinizing hormone levels. A surge in this hormone is indicative of ovulation. Once an IUI/ICI procedure is performed, it is typically repeated again within 12 hours. This helps to increase conception chances.
Procedure Steps:
Step 1: If the female is not using fertility drugs the insemination takes place between day 12 and day 16 of her menstrual cycle since ovulation is expected on or around day 14.
To identify when she is about to ovulate a series of tests and techniques may be used: the female may be taking blood or urine tests and many clinics may provide tools and information such as an ovulation predictor kit to detect the LH hormone surge, which signals imminent ovulation. Two complimentary techniques to track ovulation are temperature tracking and checking the viscosity of cervical mucus.
If the female uses fertility drugs to stimulate ovulation, the development of the eggs may be tracked by vaginal ultrasound scans. As soon as an egg is mature, she is given a hormone injection to stimulate its release.
Step 2: The sperm is inserted approximately 36 hours following ovulation. The doctor will first insert a speculum into the vagina. This is the same instrument that keeps the vaginal walls apart during the cervical smear test.
The procedure will differ slightly depend on whether it is a IUI or ICI
IUI
A small, soft, flexible catheter tube is then threaded into the womb via the cervix. This allows the prepared sperm to be inserted directly into the uterus.
This process is usually a painless procedure and will take just a few minutes. Some women may experience a temporary, menstrual-like cramping.
ICI
A syringe is inserted through the open speculum. The plunger is then pushed forward and the semen in the syringe is emptied deep into the vagina. The syringe (and speculum if used) may be left in place for several minutes.
Unlike IUI, where the semen is injected directly into the uterine cavity, during ICI the semen is not injected as deeply. When performed at home by private individuals without the presence of a professional this procedure is also sometimes referred to as intravaginal insemination (IVI)2
Step 3: At this point the female may rest for 15 to 30min before leaving the clinic. This period of rest[1]“Laurie Barclay. “Immobilization May Improve Pregnancy Rate After Intrauterine Insemination”. Medscape Medical News. Retrieved October 31, 2009.” may allow the sperm to begin travelling through the cerivical mucus towards the egg.
Step 1: The male partner will be asked to produce a sperm sample on the day of the insemination by masturbation.
Step 2: The sperm will be washed to remove the seminal fluid surrounding them. In addition, the highest quality sperm are isolated from poor quality sperm via a centrifuge.
Step 3: The sample with the cleaned, high quality sperm is ten inserted into the uterus via the catheter tube.
Success Rates
The success rate of ICI/IUI procedures depends on the couple’s fertility “profile” and their age. Most couples have a success rate of around 5-25% with each cycle. The chances will be closer to 20% if the procedure is done with fertility drugs. Probabilities are highest when the woman is under the age of 30 and the man has more than 5 million total motile sperm[2]“Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H (November 2008). “Predictive factors for pregnancy after intrauterine insemination (IUI): An analysis of 1038 cycles and a … Continue reading (TMS) per millilitre (e.g. 50 milllion total count / ml x 20% normal forms x 50% normal progression = TMS 5 million / ml.
IUI/ICI chances of pregnancy success are reduced by advanced maternal age. 38–39 year old women appear to have reasonable success during the first two cycles of IUI/ICI when combined with controlled ovarian hyperstimulation (COH) using fertility-enhancing medication.
However, women over 40 year appear not to benefit from after a single cycle of combined IUI with controlled ovarian hyperstimulation (COH/IUI). Fertility specialists therefore tend to recommend IVF treatment after one failed COH/IUI cycle for women over 40[3]“Harris, I.; Missmer, S.; Hornstein, M. (2010). “Poor success of gonadotropin-induced controlled ovarian hyperstimulation and intrauterine insemination for older women”. Fertility and … Continue reading. These recommendations also apply to ICI cycles.
Enhancing Probabilities
As with all methods to get pregnant, the probabilities of success will greatly depend on the “fertility profile” of the couple or woman. Private individuals undertaking ICI at home may also make simple mistakes due to a lack of knowledge and practise. A trained professional will improve chances, which must be seen in relative terms
ICI/IUI can be done with or without fertility drugs to boost egg production and therefore increase the chance of conceiving. The couple should discuss the risks involved in using fertility drugs and whether IUI/ICI without fertility drugs might be suitable given the individual history of the couple or recipient. A short period of ejaculatory abstinence before intrauterine insemination is associated with higher pregnancy rates[4]“Marshburn PB, Alanis M, Matthews ML, et al. (September 2009). “A short period of ejaculatory abstinence before the treatment has been shown to produce higher pregnancy rates”. Fertil. … Continue reading.
A trained fertility professional may recommend the use of a conception cap, to stop the semen from leaking back out of the vagina. This plug-like device may be inserted into the vagina after the semen has been deposited. By leaving it in place near to the entrance to the cervix for several hours, a woman may go about her usual activities while the cervical cap holds the semen in the vagina.
Occasionally, fertility clinics may suggest to insert sperm twice per treatment cycle in order to reduce the probability of missing the fertility window dictated by ovulation. However, a randomized trial of insemination following ovarian hyperstimulation involving the use of fertility medication found no difference in live birth rate between single and double intrauterine insemination[5]”Bagis T, Haydardedeoglu B, Kilicdag EB, Cok T, Simsek E, Parlakgumus AH (May 2010). “Single versus double intrauterine insemination in multi-follicular ovarian hyperstimulation cycles: a … Continue reading.
Length and Cost of Treatment
NHS (free)
The NHS in the UK may provide up to six cycles of IUI treatment at no extra cost to the customer if:
- The female partner is unable or would find it very difficult to have vaginal intercourse. A possible cause would be a physical disability.
- Either partner has a condition such as a viral infection, which can be sexually transmitted.
- The couple is in a same-sex relationship
Previously, IUI treatment on the NHS was offered if:
- A man had mild fertility problems
- A woman had mild endometriosis
- A couple had idiopathic (unexplained) infertility
However, following budget cuts to the NHS in recent years, new National Institute for Health and Care Excellence (NICE) guidelines released in 2013 state that IUI should no longer be offered in these circumstances. Instead, the couple should be advised to keep trying to conceive through regular unprotected sexual intercourse for a total of two years. After this time they may be offered in vitro fertilisation (IVF). ICI is not funded by the NHS.
PRIVATE
IUI is also available from many private fertility clinics. Costs range between £500 to £1,000 per cycle of treatment according to individual circumstances. Each treatment cycle is timed to coincide with the woman’s natural ovulation. This makes it only possible to receive one cycle of IUI treatment a month.
Private clinics often sell packages or bundles. They may, for example, offer certain free COH medication, additional sperm-enhancing treatment or a discounted additional cycle if the couple commits to three or four cycles.
Click this link to view an example price list: https://www.completefertility.co.uk/fertility_treatment_prices.php
Fertility Tourism
Due to it’s relative low cost IUI/ICI are not as common a treatment sought by fertility tourists as ICSI and IVF. The higher absolute costs of these more advanced treatment offer a higher incentive to travel to Europe in search for lower prices. IUI prices in Poland can, however, start from as low as £98 per cycle.
Bibliography

Dr. Kooner is Deputy Director of The Advanced Fertility Center of Chicago and has been a Specialist in Fertility Treatment since 1999.
As well as the areas that the clinic specialises in general, he is particularly interested in managing oocyte donation, female same-sex couples, single women having sperm donation and those considering egg freezing.
Dr. Kooner regularly speaks at fertility meetings. He has published in national journals and constantly contributes to the fertility research and publications from Advanced Fertility Center of Chicago.
References
| ↑1 | “Laurie Barclay. “Immobilization May Improve Pregnancy Rate After Intrauterine Insemination”. Medscape Medical News. Retrieved October 31, 2009.” |
|---|---|
| ↑2 | “Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H (November 2008). “Predictive factors for pregnancy after intrauterine insemination (IUI): An analysis of 1038 cycles and a review of the literature”. Fertil. Steril. 93 (1): 79–88. doi:10.1016/j.fertnstert.2008.09.058. PMID 18996517.” |
| ↑3 | “Harris, I.; Missmer, S.; Hornstein, M. (2010). “Poor success of gonadotropin-induced controlled ovarian hyperstimulation and intrauterine insemination for older women”. Fertility and Sterility 94 (1): 144–148. doi:10.1016/j.fertnstert.2009.02.040. PMID 19394605.” |
| ↑4 | “Marshburn PB, Alanis M, Matthews ML, et al. (September 2009). “A short period of ejaculatory abstinence before the treatment has been shown to produce higher pregnancy rates”. Fertil. Steril. 93 (1): 286–8. doi:10.1016/j.fertnstert.2009.07.972. PMID 19732887.” |
| ↑5 | ”Bagis T, Haydardedeoglu B, Kilicdag EB, Cok T, Simsek E, Parlakgumus AH (May 2010). “Single versus double intrauterine insemination in multi-follicular ovarian hyperstimulation cycles: a randomized trial”. Hum Reprod 25 (7): 1684–90. doi:10.1093/humrep/deq112. PMID 20457669″ |



