What is sperm morphology / % normal shapes?
Sperm morphology refers to the size and shape of sperm. Results are reported as the percentage of sperm that appear normal when semen is viewed under a microscope.
Normally up to 10% of all spermatozoa have observable defects. In some men, this percentage can be much higher. The presence of abnormally-shaped sperm will negatively affect fertility, because an such sperm cells are disadvantaged at fertilising the ovum. This will make achieving a pregnancy less likely[1]”https://www.gfmer.ch/Endo/Lectures_09/dupan.htm“, [2]”Sadler, T. (2010). Langman\’s medical embryology. (11th ed. ed.). Philadelphia: Lippincott William & Wilkins. p. 30.ISBN 978-0-7817-9069-7“.
Sperm morphology is a predictor of success in fertilising a female egg (oocyte) during in vitro fertilisation (IVF)[3]”https://www.ncbi.nlm.nih.gov/pubmed/3335257″.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
The updated WHO male fertility criteria as described in 2010 consider a sample is normal if 4% or more of the observed sperm have normal morphology[4]”https://humupd.oxfordjournals.org/content/16/3/231“. Previous to this downward revision, 14% was considered normal[5]”https://menfertility.org/learn-to-interpret-semen-analysis/“
Poor sperm morphology / % normal shapes
Teratospermia (or teratozoospermia) is the condition characterised by the presence of sperm with abnormally poor morphology, which causes male infertility.
Solutions to sperm morphology problems
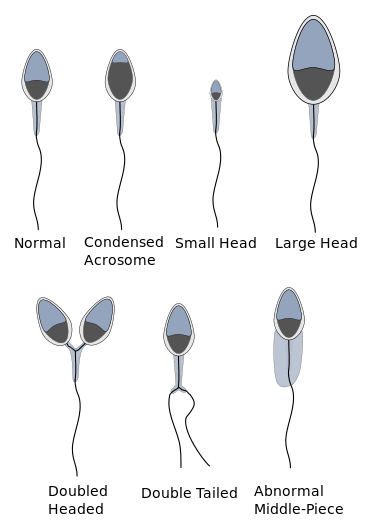
Teratospermia is diagnosed via a semen analysis, when sperm is collected and analysed under a microscope. Abnormal shapes may include heads that are large, small, tapered, duplicated or tails that are abnormally shaped such as too long or too short[6]”https://www.endotext.org/male/male7/male7_2.htm”
Antiestrogens have been shown effective in treating teratospermia[7]”https://www.gfmer.ch/Endo/Lectures_09/dupan.htm“. They blocks the production[8]”https://www.cancer.gov/dictionary/?CdrID=44813″ or utilisation of oestrogens, inhibiting their effects
Teratozoospermia can be indirectly treated by intracytoplasmic sperm injection (ICSI). The sperm cells do not need to travel, because they are injected directly into the egg[9]”French DB, Sabanegh ES, Goldfarb J, Desai N (March 2010). “Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI … Continue reading. Once the egg is successfully fertilized, poor sperm morphology does not influence blastocyst (early embryonic) development or morphology[10]”French DB, Sabanegh ES, Goldfarb J, Desai N (March 2010). “Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI … Continue reading.
Even in severe teratozoospermia, the few sperm cells that have a “normal” morphology can be detected, isolated and used for fertilisation, allowing for optimal success rate[11]”French DB, Sabanegh ES, Goldfarb J, Desai N (March 2010). “Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI … Continue reading.
In addition, teratozoospermia can be successfully treated, by supplementing the following nutrients:
- 2000 mg/day vitamin C increases sperm count 129% in 2 months[12]”https://www.ncbi.nlm.nih.gov/pubmed/17004914“
- 200 mg/day pycnogenol improves sperm morphology by 38% in 90 days[13]”https://www.ncbi.nlm.nih.gov/pubmed/12418064“
- 200 µg selenium + 400 IU Vitamin E improved motility, morphology or both in 53% of patients over 14 weeks[14]”https://www.ncbi.nlm.nih.gov/pubmed/21403799“
- Vitamin D (men low in vitamin D have lower sperm counts[15]”https://www.ncbi.nlm.nih.gov/pubmed/23042450“)
How to increase sperm shapes naturally

The sperm generation process is particularly sensitive to external factors. These include trauma (heat, physical force), energy and nutrient supply for the cells “under construction” as well as oxidative stress.
There are a number of things a man can do to improve his fertility. These include lifestyle choices such as the elimination of fast food, nicotine and alcohol, regular exercise, restful sleep and the reduction of stress.
In addition, scientific studies have show that an increase in sperm count can be achieved by taking the following food supplements:
- amino acids such as Arginine and Carnitine
- antioxidants such as Glutathione and and co-emzyme Q10
- trace metals such as zinc and selenium
- vitamins such as A, B9 (folic acid), C, D and E
- extracts such as pine bark extracts (Pycgnogenol)
These amino acids, vitamins and trace elements are naturally occurring nutrients and no side effects are to be expected. On the contrary, increasing the supply of such micronutrients causes significant health benefits such as a stabilisation of the immune system, a positive effect on cardiovascular circulation and skin and hair health.
There is therefore no medical reason not to implement a micronutrient rich diet for a minimum of six months to increase fertility. Ideally this should be carried on until successful conception.
VIDEO: Learn How To Read a Semen Analysis (video 2 of our video series)
More sperm shape-enhancing nutrients

Dr. Kooner is Deputy Director of The Advanced Fertility Center of Chicago and has been a Specialist in Fertility Treatment since 1999.
As well as the areas that the clinic specialises in general, he is particularly interested in managing oocyte donation, female same-sex couples, single women having sperm donation and those considering egg freezing.
Dr. Kooner regularly speaks at fertility meetings. He has published in national journals and constantly contributes to the fertility research and publications from Advanced Fertility Center of Chicago.
References
| ↑1, ↑7 | ”https://www.gfmer.ch/Endo/Lectures_09/dupan.htm“ |
|---|---|
| ↑2 | ”Sadler, T. (2010). Langman\’s medical embryology. (11th ed. ed.). Philadelphia: Lippincott William & Wilkins. p. 30.ISBN 978-0-7817-9069-7“ |
| ↑3 | ”https://www.ncbi.nlm.nih.gov/pubmed/3335257″ |
| ↑4 | ”https://humupd.oxfordjournals.org/content/16/3/231“ |
| ↑5 | ”https://menfertility.org/learn-to-interpret-semen-analysis/“ |
| ↑6 | ”https://www.endotext.org/male/male7/male7_2.htm” |
| ↑8 | ”https://www.cancer.gov/dictionary/?CdrID=44813″ |
| ↑9 | ”French DB, Sabanegh ES, Goldfarb J, Desai N (March 2010). “Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI cycles?”.Fertil Steril 93 (4):1097–1103. doi:10.1016/j.fertnstert.2008.10.051. PMID 19200957“ |
| ↑10, ↑11 | ”French DB, Sabanegh ES, Goldfarb J, Desai N (March 2010). “Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI cycles?”.Fertil Steril 93 (4): 1097–1103. doi:10.1016/j.fertnstert.2008.10.051. PMID 19200957“ |
| ↑12 | ”https://www.ncbi.nlm.nih.gov/pubmed/17004914“ |
| ↑13 | ”https://www.ncbi.nlm.nih.gov/pubmed/12418064“ |
| ↑14 | ”https://www.ncbi.nlm.nih.gov/pubmed/21403799“ |
| ↑15 | ”https://www.ncbi.nlm.nih.gov/pubmed/23042450“ |










I noticed that the referred abstract: “Selenium-vitamin E supplementation in infertile men: effects on semen parameters and pregnancy rate” mentions 200 micrograms instead of 200 mg as included above.
Best,
Ivonne
Thank you Yvonne, well spotted. It has been corrected.
I’ve got 3% Morphology and the other parameters are like:
count: 75 m/ml
motility: 48%
how significant is this 3% to conceive naturally?